Case Report
Magnetic Resonance Imaging Evaluation in Ischemic Priapism Secondary to Quetiapine Prescribed for Sleep Disturbance
Chelsea A Sparks, Douglas P Ivancsits and Rajendra P Kedar*
Department of Radiology, University of South Florida, Morsani College of Medicine, Tampa, Florida, USA
*Corresponding author: Rajendra P Kedar, Department of Radiology, University of South Florida, Morsani College of Medicine, Tampa, Florida, USA, Tel: +813-508-5814; E-mail: rajkedar@gmail.com
Citation: Sparks CA, Ivancsits DP, Kedar RP (2018) Magnetic Resonance Imaging Evaluation in Ischemic Priapism Secondary to Quetiapine Prescribed for Sleep Disturbance. J Clinical Case Rep Case Stud 2018: 07-10. doi:https://doi.org/10.29199/2637-9309/CCCS-102017
Received: 16 August, 2018; Accepted: 21 September, 2018; Published: 04 October, 2018
Abstract
Ischemic priapism is a low-flow state of priapism, an erection lasting >4 hours, and represents the most common subtype. It is a urological emergency which should be managed urgently to avoid complications of erectile dysfunction and fibrosis. The association of antipsychotic medications, including quetiapine, with priapism is well documented. Magnetic resonance imaging (MRI) has utility in the evaluation of fibrosis and the viability of the corpora cavernosa in ischemic priapism, in cases where ultrasound findings may be difficult to interpret, and in cases of prolonged ischemic priapism. We present a case of recurrent ischemic priapism secondary to quetiapine prescribed for sleep disturbance with associated penile ultrasound and MRI findings.
Keywords: Ischemic priapism; Magnetic resonance imaging; Quetiapine
Introduction
Priapism is a persistent penile erection continuing beyond 4 hours following or independent of sexual stimulation [1] Priapism may be categorized into three subtypes, ischemic, nonischemic, and stuttering. Ischemic priapism represents the most common subtype, accounting for 95% of priapism cases with an incidence of 0.34-1.5 per 100,000 person years [2]. Ischemic priapism is veno-occlusive or low flow in etiology and painful. There is little to no cavernosal blood flow, and cavernosal blood gases typically demonstrate hypoxia, hypercarbia, and acidosis. Ischemic priapism may result from hemoglobinopathies, hyperviscosity, thrombophilic states, or drug reactions [3]. Ischemic priapism is a compartment syndrome requiring treatment as a urological emergency to prevent erectile dysfunction and progressing fibrosis of the cavernosal tissues [1]. Nonischemic priapism is characterized by unregulated cavernosal arterial inflow [3]. In contrast to ischemic priapism, nonischemic priapism is not painful or fully rigid, does not demonstrate blood gas abnormalities, and is not a urological emergency [1]. Stuttering priapism is defined by recurrent episodes of painful and self-limiting erections which last <4 hours [4]. Mechanistically, stuttering priapism is similar to ischemic priapism [4].
Ischemic priapism may be further investigated through imaging. Penile doppler ultrasound will demonstrate the absence of flow within the dorsal penile arteries and corpora cavernosa [5]. Magnetic resonance imaging (MRI) is useful in evaluating priapism as it can identify the presence of fibrosis and may be used to assess the viability of the corpora cavernosa [6]. European Association of Urology (EAU) guidelines recommend MRI evaluation in cases of prolonged ischemic priapism given its 100% sensitivity in predicting non-viable smooth muscle [7]. MRI has greater utility after multiple aspirations of the corpus cavernosa or surgical shunting procedures. These interventions may cause ischemic priapism to resemble high flow, nonischemic priapism on ultrasound and result in patchy areas of reperfusion [5]. Typical MRI findings include non-enhancement of the corpus cavernosa with strong enhancement of the corpus spongiosum post contrast [6].
Priapism is a known uncommon side effect of antipsychotic drugs and quetiapine, an atypical antipsychotic, has been indicated in several cases of priapism [8]. Quetiapine has α 1 and α
1 and α 2 receptor antagonistic activity which is thought to contribute to its association with priapism [8]. Here, we present a case of recurrent priapism with resulting ischemia in a patient on quetiapine. This case demonstrates the prototypical radiographic features of ischemic priapism on MRI.
2 receptor antagonistic activity which is thought to contribute to its association with priapism [8]. Here, we present a case of recurrent priapism with resulting ischemia in a patient on quetiapine. This case demonstrates the prototypical radiographic features of ischemic priapism on MRI.
Case Report
A 36-year-old man with a history of a single unprovoked and self-resolving episode of priapism ten years ago, presented to the emergency department with a painful erection lasting >48 hours. The erection was persistent, despite seeking care at an outside emergency department earlier that day where he received penile epinephrine and saline injections. Additionally, he reported multiple episodes over the two weeks before his arrival, which resolved after saline and phenylephrine injections at outside facilities. For the past month, he endorsed taking quetiapine 100 mg for sleep disturbance. He did not have a history of sickle cell disease. Physical exam was significant for an erect penis with bruising at the base bilaterally. He continued to endorse penile pain at the time of the examination.
Penile epinephrine and saline injections in the emergency department failed to provide improvement. Complete blood count and basic metabolic panel were unremarkable. An air-blood gas was obtained which demonstrated pO2 29 mmHg, pCO2 68 mmHg, and pH 7.00, suggestive of penile ischemia. Urology was consulted. An MRI pelvis without and following ten mL of MultiHance IV contrast was performed to evaluate for necrosis, quality of smooth muscle, and corporal body viability per urology secondary to his prolonged and refractory priapism.
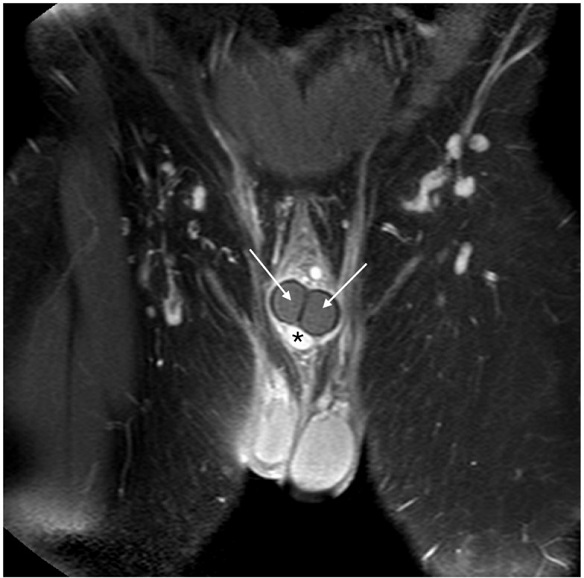
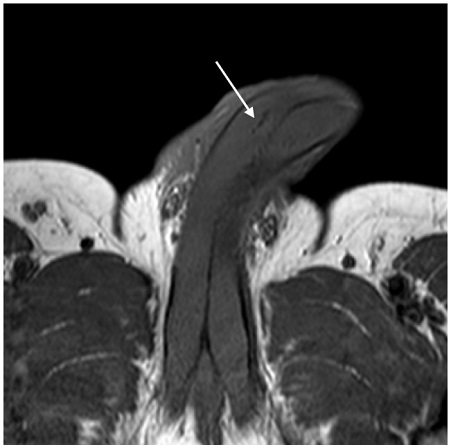
MRI demonstrated subcutaneous soft tissue edema along the hyperemic penile shaft (Figure 1). The enhancement pattern of the corpus spongiosum was normal. There was a near complete absence of normal enhancement of the corpora cavernosa (Figure 2). Minimal serpiginous enhancement within the right corpus cavernosum at the base most likely reflected minimal perfusion surrounding the cavernosal artery. There were non-enhancing foci of T1 and T2 signal hypointensity within the corpus cavernosum distally on the right, felt to correspond to suspected gas foci. These were likely related to penile aspiration performed at an outside facility or developing necrosis (Figure 3). The findings were consistent with diffuse cavernosal infarction bilaterally with associated edema and hyperemia within the penile subcutaneous soft tissues.
|
Figure 1: Short TI Inversion Recovery (STIR) sagittal section. There is subcutaneous and soft tissue edema along the penile shaft. |
|
Figure 2: Post contrast coronal section demonstrating non-enhancement of the corpora cavernosa (arrows) and normal enhancement of the corpus spongiosum (asterisk). |
|
Figure 3: T1 weighted axial section. There is a non-enhancing focus of T1 hypointensity within the right corpus cavernosum. |
|
Figure 4: Transverse doppler ultrasound of the penis demonstrating non-visualization of the dorsal penile or caversonal arteries. Echogenic foci likely representing post-procedural gas are present (arrows). |
Surgical options were discussed with the patient. He elected for surgical shunting over the immediate placement of a penile prothesis. Detumescence was not achieved following Winters shunt placement but was successful with corporal snake shunt, which resulted in the improvement of his pain. His postoperative course was complicated by residual penile fibrosis after detumescence. He has since followed with urology on an outpatient basis, has no residual penile pain, and has discontinued quetiapine. There have been no episodes of priapism in the three months following his discontinuation of quetiapine. He is scheduled to undergo placement of a semi-rigid penile prothesis secondary to residual fibrosis of the corpora.
Discussion
Priapism is defined as an erection lasting >4 hours and encompasses three subtypes. Ischemic priapism is a low-flow or veno-occlusive subtype and represents 95% of priapism cases. It should be managed emergently to avoid erectile dysfunction and progressing fibrosis of the cavernosal tissues [1]. It usually presents clinically with fully rigid corpora cavernosa, penile pain, and abnormal cavernous blood gases [1]. The etiology of ischemic priapism includes drugs, particularly antipsychotics, hematological disorders, and metabolic disorders [9]. This patient demonstrated physical exam findings and laboratory abnormalities of ischemic priapism. His blood gas was characterized by hypoxia, hypercarbia, and acidosis. While his repeated episodes may suggest stuttering priapism, he does not meet criteria, as the episodes were >4 hours in duration and were not self-limiting, requiring interventional management to resolve each occurrence [4].
Urgent management is critical to avoid complications in ischemic priapism and treatment typically follows a stepwise approach. Decompression with aspiration is usually attempted first, followed by intracavernous injections of a sympathomimetic drug if unsuccessful [7]. These procedures may be repeated before attempting to achieve detumescence by surgical means in the event of continued treatment failure. Surgical shunt procedures and implantation of a penile prothesis, in cases of priapism >36 hours or in which all other interventions have failed, may be pursued as the next steps in management [7]. Management via sympathomimetic agents was unsuccessful for this patient at the outside facility and when he presented. Given the duration of his most recent episode of priapism, he would have been a candidate for immediate placement of a penile prothesis. However, he elected to proceed with surgical shunting and detumescence was successful through a snake shunt maneuver. A corporal snake shunt is a maneuver in which a dilator is inserted via a retrograde approach into each corporal body through a transverse glandular incision and gently advanced several centimeters to facilitate the release of congested blood [10]. Despite successful detumescence, this patient experienced residual penile fibrosis for which he will ultimately undergo implantation of a penile prothesis. This patient’s multiple refractory episodes requiring interventional management and most recent episode duration of >48 hours were likely contributing factors to his development of fibrosis.
The development of priapism on quetiapine is a well-established phenomenon within the literature, typically occurring in patients with schizoaffective disorder or schizophrenia [11-13]. It has been reported following a single dose of quetiapine for insomnia [14]. Priapism has also been reported to occur with concomitant use of quetiapine and other substances, such as recreational amphetamines [15]. Recurrent priapism with the use of quetiapine has been documented with the concurrent use of cocaine and in patients with schizoaffective disorder [12,16,17]. This case is the first of recurrent priapism requiring multiple interventions on quetiapine alone in a patient without schizoaffective disorder. This patient’s remote history of priapism may have predisposed him to develop this rare side effect of quetiapine on multiple occasions. This case also represents the first report of ischemic priapism on quetiapine in which MRI findings are presented concomitantly.
Although MRI is not routinely used in the diagnosis of acute ischemic priapism, it remains a valuable imaging modality in difficult cases when multiple aspirations from the corpora cavernosa or surgical shunt procedures have been completed. These manipulations can hinder ultrasound evaluation by causing low-flow priapism to resemble high-flow on imaging [5]. MRI may also be employed to determine corpora cavernosa viability and fibrosis [6]. MRI findings have demonstrated a high correlation with histological analysis, predicting non-viable smooth muscle with 100% sensitivity [5]. In cases of prolonged ischemic priapism, the EAU recommends MRI evaluation for prediction of smooth muscle viability as well as to confirm erectile function restoration [7]. The patient, in this case, was a suitable candidate for MRI evaluation, given his history of intervention at an outside facility before presentation and priapism lasting >48 hours. This case demonstrates the prototypical and salient findings of ischemic priapism on MRI of the pelvis. MRI in ischemic priapism should demonstrate low signal intensity in the corpus cavernosum and normal high-intensity signal in the corpus spongiosum [9]. There will be no enhancement of the corpora cavernosa on T1 or T2 weighted images post gadolinium administration.
Conclusion
Ischemic priapism is the most common priapism subtype and is a compartment syndrome, requiring emergent treatment to avoid complications such as erectile dysfunction or cavernosal fibrosis. The role of MRI in the acute diagnosis of ischemic priapism has yet to be fully established [5]. However, it is recommended in the evaluation of prolonged ischemic priapism [7]. MRI is useful in assessing fibrosis and the viability of the corpora cavernosa in prolonged ischemic priapism, establishing its utility for future management. MRI should not be discounted as a viable imaging modality in difficult diagnostic cases or when the development of future recommendations is desired, particularly in cases of prolonged ischemic priapism. Prototypical features of ischemic priapism on MRI include loss of T1 and T2 signal in the corpora cavernosa with no gadolinium enhancement.
Conflict of Interest
All authors have no conflicts of interest to disclose.
References
- Montague DK, Jarow J, Broderick GA, Dmochowski RR, Heaton JP, et al. (2003) American Urological Association Guideline on the Management of Priapism. J Urology 170: 1318-1324.
- Ridgley J, Raison N, Sheikh MI, Dasgupta P, Khan MS, et al. (2017) Ischaemic priapism: A clinical review. Turk J Urol 43: 1-8.
- Berger R, Billups K, Brock G, Broderick GA, Dhabuwala CB, et al. (2001) Report of the American Foundation for Urologic Disease (AFUD) Thought Leader Panel for evaluation and treatment of priapism. Int J Impot Res 13: S39-S43.
- Raslan M, Hiew K, Hoyle A, Ross DG, Betts CD, et al. (2016) Surgical Management of Stuttering Ischemic Priapism: A Case Report and Concise Clinical Review. Urol Case Rep 16: 22-24.
- Ralph DJ, Borley NC, Allen C, Kirkham A, Freeman A, et al. (2010) The use of high-resolution magnetic resonance imaging in the management of patients presenting with priapism. BJU Intl 106: 1714-1718.
- Kirkham APS, Illing RO, Minhas S, Allen C (2008) MR Imaging of Nonmalignant Penile Lesions. Radiographics 28: 837-853.
- Hatzimouratidis K, Giuliano F, Moncada A, Salonia A, Verze P (2016) EAU Guidelines on Erectile Dysfunction, Premature Ejaculation, Penile Curvature, and Priapism. European Association of Urology: 46.
- Sood S, James W, Bailon MJ (2008) Priapism associated with atypical antipsychotic medications: a review. Int Clin Psychopharmacol 23: 9-17.
- Sadeghi-Nejad H, Seftel AD (2002) The etiology, diagnosis, and treatment of priapism: a review of the American Foundation for Urologic Disease Consensus Panel Report. Curr Urol Rep 3: 492-498.
- Burnett AL, Pierorazio PM (2009) Corporal “Snake” Maneuver: Corporoglandular Shunt Surgical Modification for Ischemic Priapism. J Sex Med 6: 1171-1176.
- Du Toit RM, Millson RC, Heaton JP, Adams MA (2004) Priapism. Can J Psychiatry 49: 870-871.
- Saghafi O, Kao A, Druck J (2014) Recurrent Priapism from Therapeutic Quetiapine. West J Emerg Med 15: 114-116.
- Sinkeviciute I, Kroken RA, Johnsen E (2012) Priapism in Antipsychotic Drug Use: A Rare but important Side Effect. Case Reports in Psychiatry.
- Ozkaya F, Ziypak T, Adanur S, Yucel A, Aydinoglu U (2012) The Occurrence of Priapism as a Result of the Use of a Single Dose of Quetiapine. Eurasian J Med 44: 122-123.
- Harrison G, Dilley JW, Loeb L, Nelson K (2006) Priapism and quetiapine: a case report. Psychopharmacol Bull 39: 117-119.
- Tsai AC (2011) A Case of Recurrent Priapism in the Context of Quetiapine Use, Discontinuation, and Rechallenge. J Clin Psychopharm 31: 235-236.
- Jackson JC, Torrence CL (2015) Quetiapine-induced Priapism Requiring Frequent Emergency Admissions: A Case Report. Urol Case Rep 3: 1-2.
 LOGIN
LOGIN REGISTER
REGISTER.png)