Case Study
An Already Rare Malignant Solitary Fibrous Tumor of the Prostate With Metastasis to the Lung: A Case Report, and Review of the Literature
Ahmed M El Farrah*
Palm Springs Hospital, Miami, Florida, USA
*Corresponding author: Ahmed M El Farrah, Palm Springs Hospital, Palm Springs, California, USA, Tel: 1 (305) 558-2500 ext. 4719; E-mail: amelfa256@gmail.com
Citation: El Farrah AM (2018) An Already Rare Malignant Solitary Fibrous Tumor of the Prostate With Metastasis to the Lung: A Case Report, and Review of the Literature. Case Report and Literature Review. J Clinical Case Rep Case Stud 2018: 01-06. doi: https://doi.org/10.29199/2637-9309/CCCS-102016
Received: 18 October, 2017; Accepted: 16 May, 2018; Published: 27 June, 2018
Abstract
This is the 23rd ever reported SFT of the prostate, and of the 22 others, the 5th metastatic SFT reported. We report this rare case in a 72-year-old male presenting with intermittent urinary retention and constipation. Our research lead us to a unique case of an already rare SFT in the prostate, as well as remarkably 'multiple first's' that have never been considered or reported within the current literature. A Solitary fibrous tumor (SFT), also known as fibrous tumor of the pleura, is a rare mesenchymal type tumor usually originating in the pleura and rarely any soft tissue site including the seminal vesicle. About 85% of SFT's are benign (conventional) and 15% are metastatic (malignant). Somatic fusions of four gene types, STAT6 located at chromosomal region 12q13, and the other three bcl-2, CD99, and CD34 (mostly conventional type) have been identified in solitary fibrous tumors. Currently, the treatment of choice for both conventional and malignant SFT's is surgical resection. The prognosis in conventional SFTs is excellent, but in malignant SFTs it much more guarded. About 60% of patients will have a recurrence of their tumor in which more than half the recurrence will lead to their demise within 2 years. Currently, chemotherapy and/or radiotherapy in malignant SFT’s remain controversial.
Keywords: Solitary fibrous tumor; Benign; Malignant; Prostate tumor
Introduction
Most SFTs occur in adults, with a median age of 45-50 years. SFT is less common in infants and children. Soft-tissue SFTs represent only about 1-2% of all soft-tissue tumors [1]. SFTs are tumors of mesenchymal origin that occur in the extremities. According to the updated classification of soft-tissue tumors [2,3]. Malignant forms of SFT are defined as hyper cellular, mitotically active (>4 mitoses/10 high-power fields), and characterized by cytologic atypia, tumor necrosis, or infiltrative margins [3]. A single-center study found that malignant SFT, as compared with benign SFT, was associated with larger tumors, elevated mitotic counts, the presence of metastases at diagnosis, and more extensive use of chemotherapy and radiation therapy [4]. Solitary fibrous tumor is an uncommon soft tissue neoplasm with intermediate biological behavior, which rarely metastasizes. Malignant solitary fibrous tumor, although not clearly defined, is rarely described in the prostate. This tumor typically spreads via hematogenous dissemination, primarily to the lungs, but rarely spreads via the lymphatics. Metastatic disease is usually the cause of death. Metastasis appears to be more likely an aggressive SFT of extra thoracic origin than with thoracic SFT [4]. Other aggressive soft tissue thoracic sarcomas like hemangipericytoma (HPC) are also likely in the more traditional cases. A hemangiopericytoma is a type of soft tissue sarcoma that originates in the pericytes in the walls of capillaries. As stated before SFT’s are of soft tissue origin. When HPC’s are inside the nervous system, although not strictly a meningioma tumor, it is of a meningeal origin with a special aggressive behavior. Conventional SFT's and HPC's have a better prognosis than some older studies may suggest, in that these studies may have inadvertently included sarcomas with HPC-like features. For patients with a primary tumor who undergo complete resection, 5-year survival is 89-100%. For patients with SFTs of an extremity, the local recurrence rate is 0-6%, and the distant metastasis rate is 0-19% [2,5,6,7].
Case Presentation
This is a 72-year-old Greek Male with an initial presentation of intermittent urinary retention and constipation. His risk factors such as age and genetic predisposition’s along with a thorough history and physical, DRE, and PSA warranted an ultrasound. The initial diagnosis was an enlarged prostate from benign enlargement. The findings from the physical exam, labs, and imaging were peculiar to presentation of intermittent retention. The symptoms were semi-controlled with medication, and the option of cathertization wasn't considered. The findings lead towards management with elective procedures for benign enlargement of the prostate. Management options were discussed with the patient and the urologist elected to utilize a Green light (form of TURP) fulgurating 200 cc's of the prostate which did not alleviate the symptoms, the irony of removing 200 cc's and not alleviating symptoms lead the first urologist to refer the patient to another urologist for a second opinion. The first step in management by the second urologist was obtaining a PSA with imaging. The patients PSA was 0.344 and imaging on CT showed a mass on the lung and an enlarged prostate of 16.1cm × 11.3cm × 17.3cm (1,637 cc's) with the 17.3 cm aspect of the prostate growing cranio-caudal into the bladder and lateral to the urethra. This finding raised a suspicion to the second urologist that this might not be from benign enlargement causing intermittent retention. Biopsies were now warranted to determine tissue type and possibility of malignancy. The patient was set up for an elective surgical procedure for biopsies, and 32 specimens from the twelve different cores were collected for pathological analysis. 32 specimens were obtained because of the enormous size and to make sure there were plenty of samples to rule in or out malignancy. The pathology report came back that reported solitary fibrous tumor with metastasis. The prostate tissue was STAT6 (-) and desmin (-) and, CD34, bcl2 and CD99 (+) which are markers for the specific tissue type, but indirectly diagnosed by its metastasis to the lung tissue that showed STAT6 (+) and also indirectly desmin (-). Pathology also reported that the now diagnosed 'metastatic solitary fibrosis' SFT prostate was a densely packed mass comprising of 93% malignant tissue. The final pathological conclusions were consistent with the diagnosis of a Malignant Solitary Fibrous Tumor of the Prostate, with spindle cell formations, the first ironically found in the United States of America instead of a more common presentation or place reported with this tumor type. Due to the diagnosis and the manifestation clinically of the patient, conventional management with wide surgical resection was deferred and management with chemotherapy and radiation was instead utilized. This unconventional management extended him to an almost three year (54 month) comfortable quality of life up to his demise.
Discussion
Solitary Fibrous Tumors (SFT's) are rare neoplasm's of mesenchymal origin that should be considered in cases of prostatic tumor with a spindled morphology. Positive nuclear staining for STAT6 is currently the most accurate diagnostic test. Also, for accurate diagnosis of SFT's of the prostate, immunohistochemistry is always necessary. In the setting of differentiating prostatic SFT's from different tissue types, the most helpful markers are SMA, desmin, CK, CD117, CD34, PgR, bcl 2 and CD99 along with STAT6. Diagnosis of SFT has classically been based on the immunohistochemically expression of the three initial markers CD34, bcl2 and CD99. Nevertheless, recent studies have demonstrated the poor specificity of these markers [6]. CD34 is expressed significantly in a large number of soft tissue neoplasms and many entities that are included in the differential diagnosis of SFT, such as PSS and GIST, share CD34 expression [7]. Furthermore CD34 expression is absent in approximately 5–10% of conventional SFT and in the large majority of malignant and dedifferentiated forms [7,8]. Therefore the absence of CD34 expression does not exclude the diagnosis of SFT. The expression of Bcl2 and CD99 are variably used to support the diagnosis of SFT but are less sensitive than CD34 and equally non-specific [9]. Recently, the discovery of the NAB2-STAT6 fusion gene in SFT led to development of a STAT6 antibody that is a reliable immunohistochemical marker with a high level of sensitivity and specificity [9-29]. Therefore, nuclear expression of STAT6 is currently the most useful marker for distinguishing SFT from its histologic mimics. STAT6 nuclear expression has been demonstrated both in conventional and in malignant SFT, while dedifferentiated forms frequently lose STAT6 expression [10]. Most patients with SFT's and HPC's have a benign clinical course, but because of the lesion's malignant potential, wide resection and careful longterm follow-up are necessary. Favorable long-term outcomes have been reported in cases of intracranial SFT that required repeat radiosurgery [10]. Current literature states, in regards to the more aggressive malignant SFT tissue types, there tend to be higher rates of local recurrences and distant metastasis [11]. As per current literature, despite wide surgical excision, estimated recurrence rate for malignant SFT is approximately 30% [11]. Conventional management for wide surgical excision is stated to be the most important prognostic factor. The current conventional management methods also state that the prognosis is worse in patients with metastatic disease, with median survival ranging from 22 to 46 months [11]. For unresectable disease, chemotherapy and radiation therapy showed variable efficacy [12]. For this newly reported case having a malignant solitary fibrosed tissue type and unconventional method for diagnosing and elective management of chemotherapy and radiation instead of wide surgical resection, improved the patient’s quality of life and extended his life past the high end of the median survival of 46 months to 54 months. The reasoning behind wide surgical resection thus far is that even the benign-appearing solitary fibrous tumors (SFTs) can be locally recurrent and metastatic so wide resection is the current recommendation for both benign and malignant SFTs. Further recommendations for preoperative vascular studies and arterial embolization should also be considered due to the known bleeding risk with resection [13,19]. Careful exclusion of other diagnoses (e.g. synovial sarcoma) is important. Because of the favorable outcome with SFTs, it may be possible to avoid limb-threatening and deforming operations [14]. Until this reported case, no evidence suggests that adjuvant chemotherapy is beneficial, and for SFT with malignant histologically, adjuvant radiation therapy may be considered and long-term follow-up is recommended because local and distant relapse is possible, even with benign-appearing tumors. This is the 23rd ever reported SFT of the prostate, and of the 22 others, the 5th metastatic SFT reported. This 72-year-old male presenting with intermittent urinary retention and constipation is not only an already rare SFT in the prostate but also has remarkably 'multiple first's' that have never been considered or reported within the current literature. This case of SFT was found in the United States of America, instead of a more common presentation or places like Europe and Asia reported with this tumor type. To start, the PSA value of 0.344 was virtually undetectable for his age, size of the prostate with malignant potential. This current reported case is contrary to the documented elevated PSA's from previous similar cases. The 22 other reported cases all had PSA's above 1 with the largest or most significant ones recorded having PSA's of 3-5. This patient PSA is the lowest of the 22 reported cases, which also from initial clinical diagnosing and management methods, doesn't necessarily throw up 'Red Flags' especially at his advanced age. From the 22 cases reported, this case is also the largest reported of 1197 cc's minus 200 cc's of fulgurated tissue by Green light (TURP). Comparing this now largest prostatic tissue type with the next largest, the 3 axis are anterior/posterior, transverse and cranio-caudal. Up to this point within the current literature, this tumor has been shown to be the largest one found with dimensions of 16.1cm × 11.3cm × 17.2cm (Figure 1). This particular prostate cranio-caudal measurement was 17.3 cm, even after fulguration of 200 cc's, the other two dimensions anterior/posterior and transverse were 16.1 cm and 11.3 cm, the next largest was reported at 20cmx 10cm with 20cm being transverse and the 10cm was either of anterior/posterior or cranio-caudal axis. [15]. Looking at the data now, the low PSA, DRE, and the growth of the prostate adjacent to the urethra at the bladder outlet in a cranio-caudal fashion possibly caused the intermittent retention and constipation leading the diagnosis toward benign enlargement. Most of the other reported cases the transverse growth possibly lead their ultimate diagnosis with obstructive symptoms, more cases are needed to see if this is a trend. Also noteworthy is the unique approach with the 32 specimens and obtaining the definitive diagnosis of a Solitary Fibrous tumor. The specific marker's for diagnosing the SFT weren't detectable or not accurate to traditional diagnoses. A more indirect approach, which was also contrary to the direct approaches of the other 22 reported. Being that this is the 23rd ever reported solitary fibrous tumor and the 5th only to metastasize, from current literature, the STAT6 is one of the best markers to make the diagnosis [15]. In a unique fashion this particular solitary fibrous tumor was STAT6 (-) but indirectly diagnosed by its metastasis to the lung that showed STAT6 (+) in the lung (Figure 2). The current literature also says the CD34 marker is usually absent in 5-10% of Solitary Fibrosis Tumors SFT, and if positive usually indicates the Conventional Solitary Fibrosis tissue type [16]. This solitary fibrous tumor has a CD34 (+) and Metastatic Solitary Fibrosis type. This particular tumor also had bcl2 and CD99 which make this tumor common to the total reported 22 to date solitary fibrous tissue types [16, 17]. The other indirect link to the pathological marker diagnosis was finding desmin (-) which differentiated this tumor from the Smooth Muscle Fibrosis type SMF. The final pathological conclusions were consistent with the diagnosis of a Malignant Solitary Fibrous Tumor of the Prostate, with spindle cell neoplastic tissue. Also, with this particular SFT, it is currently the most densely packed mass of the malignant type ever reported. The analysis of the 32 specimens collected reported the area of 'metastatic solitary fibrosis' at 93% replacing all prostatic parenchyma compared to the next closest reported case encompassing only 50% of the prostatic parenchyma. The unconventional management of the patient was paramount and differed from the 22 reported cases and the 4 of them that metastasized conventional management called for wide surgical resection, which is the preferred method and the best prognostic factor [18]. Up until this particular case, there really hasn't been any metastatic disease to study from or its management due to the already rarity of the tumor type and its location. Wide surgical Resection was not utilized, but instead chemotherapy and routine radiation treatment’s which helped improve his quality of life and extended him past the two-year prognostic factor that has only been reported in the four metastatic types of this particular tumor. Chemotherapy was warranted because of metastatic disease, the next largest reported case to this diagnosis, as previously stated, had 50% malignant type tissue but never metastasized; therefore, the mass was resected. Of all of the SFT prostate cases reported, if the prostate was large enough, conventional treatment was resection, the smaller ones were managed with chemotherapy and radiation. This current prostate was large and of metastatic nature which required chemotherapy and radiation. The 4 metastatic SFT's ever reported, died shortly after resection. Because the conventional management method with surgical and instrument resection was deferred, and the unconventional option of chemotherapy and radiation was utilized, this unconventional management option improved his quality of life and extended his life expectancy longer than any known reported case.
|
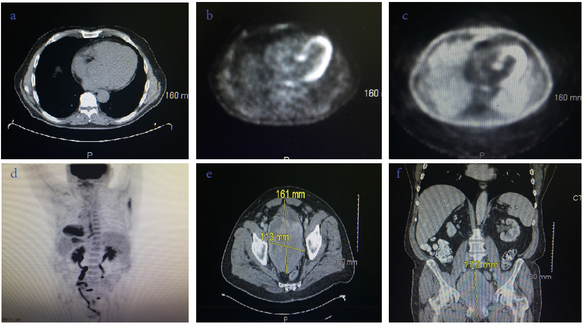
Figure 1: a. Transverse CT without contrast showing lung mass in the left thoracic cavity. b. Transverse PET scan without contrast showing lung mass in the left thoracic cavity. c. Transverse PET scan with contrast showing enhanced borders of the lung mass in the left thoracic cavity. d. A/P PET scan results showing STAT 6 (+) Metastasis to the prostrate. e A/P, Tranverse, and Cranio-Caudal CT with dimensions of Solitary Fibrous Tumor of the Prostate. |
|
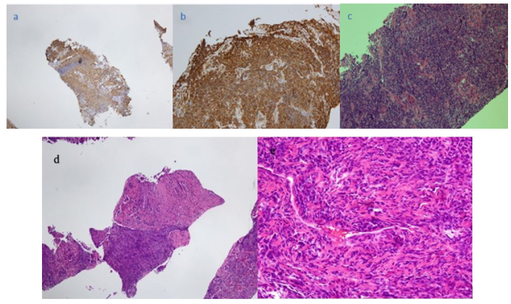
Figure 2: a) STAT 6 (-) Prostate tissue. b) CD 34 (+) Prostate tissue. c) Stat 6 (+) Lung tissue. d) Alternating hypo-cellular and hyper-cellular areas of malignancy with demarcated border e) Hyper-cellular areas with patch-less population of ovoid cells and spindle formations |
Conclusion
Compared to similar 'Solitary Fibrous like' malignancies, this is the 23rd ever reported case, and the 5th to ever metastasize, and multiple first's reported with its unique presentation found in the United States. Initially, due to the presentation of intermittent retention, PSA of 0.344, and imaging showing enlargement, medicines and elective procedures were warranted, and when these didn’t correlate, further imaging and biopsies painted a better picture of what was going on. The irony of the presenting symptoms of intermittent retention instead of obstruction that delayed the definitive diagnosis is worth investigating in the future. Acquiring more data is needed to differentiate obstructive symptoms from transverse growth of the prostate vs. intermittent retention symptoms from growth of the prostate cranio-caudal into the bladder adjacent to the urethra. This data possibly can help with arriving at quicker definitive diagnoses, proper management and efficient utilization of resources, and improving the conventional management and quality of life in patients with this rare prostatic tissue type. The unconventional method for diagnosing the SFT by STAT 6 (+) in the metastatic lung tissue and desmin (-) in the prostatic tissue should be further investigated and possibly utilized in the known conventional methods as data is slowly obtained for this already rare prostatic tissue type. Also, this the first case reporting the Malignant Solitary Fibrous Tumor type of 93%. Being that it is the largest and most densely packed with malignant tissue type, the unconventional approach utilized that improved the patient’s quality of life and mortality should be considered as more conventional managing methods as this rare tissue type surfaces in the future. This case presentation hopefully of brings awareness of diagnosing tumor types utilizing unconventional methods and indirect approaches especially in the rarest forms and tissue types. Also, this case presentation is to bring awareness of the management option that to date allowed the patient to live longer and to the best quality of life possible as his disease progressed. This management option also is suggested if future rare tumor processes of this type occur in the future. Further data for already rare SFT's of the prostate are needed to strengthen this unconventional method for diagnosing and managing the tumor type.
Acknowledgements
Dr. Darwich Bejany MD, and Dr. Merce Jorda MD, University of Miami.
Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Conflict of Interest
The authors declared no potential conflict of interests with respect to the research authorship, and/or publication of this paper.
Funding
The work on the present paper was not funded by any source.
References
- Penel N, Amela EY, Decanter G, Robin YM, Marec-Berard P (2012) Solitary fibrous tumors and so-called hemangiopericytoma. Sarcoma. 2012: 690251.
- Espat NJ, Lewis JJ, Leung D, Woodruff JM, Antonescu CR, et al. (2002) Conventional hemangiopericytoma: modern analysis of outcome. Cancer. 95: 1746-1751.
- Fletcher CDM, Bridge JA, Hogendoorn P, Mertens F (2013) WHO Classification of Tumours, Volume 5: WHO Classification of Tumours of Soft Tissue and Bone (4th edn). Geneva: WHO Press.
- DeVito N, Henderson E, Han G, Reed D, Bui MM, et al. (2015) Clinical Characteristics and Outcomes for Solitary Fibrous Tumor (SFT): A Single Center Experience. PLoS One 10: e0140362.
- O'Neill AC, Tirumani SH, Do WS, Keraliya AR, Hornick JL, et al. (2017) Metastatic Patterns of Solitary Fibrous Tumors: A Single-Institution Experience. AJR Am J Roentgenol 208: 2-9.
- Miettinen M (2014) Immunohistochemistry of soft tissue tumours - review with emphasis on 10 markers. Histopathology 64(1): 101–118.
- Demicco EG, Park MS, Araujo DM, Fox PS, Bassett RL, et al. (2012) Solitary fibrous tumor: a clinicopathological study of 110 cases and proposed risk assessment model. Mod Pathol 25: 1298- 1206.
- Paner GP, Aron M, Hansel DE, Amin MB (2012) Non-epithelial neoplasms of the prostate. Histopathology 60: 166–186.
- Akisue T, Matsumoto K, Kizaki T, Fujita I, Yamamoto T, et al. (2003) Solitary fibrous tumor in the extremity: case report and review of the literature. Clin Orthop Relat Res 236-244.
- Lorigan JG, David CL, Evans HL, Wallace S (1989) The clinical and radiologic manifestations of hemangiopericytoma. AJR Am J Roentgenol 153: 345-349.
- Cheville J, Algaba F, Epstein JI, Lopez-Beltran A (2016) In: Moch H, editor. WHO classification of tumours of the urinary system and male genital organs (4th edn). Lyon: the International Agency for Research on Cancer press p: 177.
- Arce-Lara C, Shah MH, Jimenez RE, Patel VR, Benson DM Jr, et al. (2007) Gastrointestinal stromal tumors involving the prostate: presentation, course, and therapeutic approach. Urology 69: 1209.
- Lococo F, Cesario A, Cardillo G, Filosso P, Galetta Da, et al. (2012) Malignant solitary fibrous tumors of the pleura: retrospective review of a multicenter series. J Thorac Oncol 7: 1698–1706.
- Khalifa J, Ouali M, Chaltiel L, Le Guellec S, Le Cesne A, et al. (2015) Efficacy of trabectedin in malignant solitary fibrous tumors: a retrospective analysis from the French sarcoma group. BMC Cancer 15: 700.
- Ronchi A, La Mantia E, Gigantino V, Perdonà S, De Sio M, et al. (2017) A rare case of malignant solitary fibrous tumor in prostate with review of the literature. Diagn Pathol 12: 50.
- Yang W, Sun F, Liu H, Wang G, Shi P, et al. (2015) Solitary fibrous tumors of the prostate: a case report. Oncology Letters 10: 1617–1619.
- Yoshida, K. Tsuta, M. Ohno, Yoshida M, Narita Y et al. (2014) STAT6 immunohistochemistry is helpful in the diagnosis of solitary fibrous tumors. Am J Surg Pathol 38: 552–559.
- Doyle LA, Vivero M, Fletcher CD, Mertens F, Hornick JL (2014) Nuclear expression of STAT6 distinguishes solitary fibrous tumor from histologic mimics. Modern Pathol 27: 390–395.
- Mosquera JM, Fletcher CD (2009) Expanding the spectrum of malignant progression in solitary fibrous tumors: a study of 8 cases with a discrete anaplastic component--is this dedifferentiated SFT? Am J Surg Pathol 33: 1314–1321.
- Herawi M, Montgomery EA, Epstein JI (2006) Gastrointestinal stromal tumors (GISTs) on prostate needle biopsy: a clinicopathologic study of 8 cases. Am J Surg Pathol 30: 1389–1395.
- Hansel DE, Netto GJ, Montgomery EA, Epstein JI (2008) Mesenchymal tumors of the prostate. Surg Pathol Clin 1: 105–128.
- Gaudin PB, Rosai J, Epstein JI (1998) Sarcomas and related proliferative lesions of specialized prostatic stroma: a clinicopathologic study of 22 cases. Am J Surg Pathol 22: 148–162.
- Hossain D, Meiers I, Qian J, Mac Lennan GT, Bostwick DG (2008) Prostatic stromal hyperplasia with atypia: follow-up study of 18 cases. Arch Pathol Lab Med 132: 1729–1733.
- Hossain D, Meiers I, Qian J, Mac Lennan GT, Bostwick DG (2008) Prostatic leiomyoma with atypia: follow-up study of 10 cases. Ann Diagn Pathol 12: 328–332.
- Masuda Y, Kurisaki-Arakawa A, Hara K, Arakawa A, Oh S, et al. (2014) A case of dedifferentiated solitary fibrous tumor of the thoracic cavity. Int J Clin Exp Pathol 7: 386–393.
- Kurisaki-Arakawa A, Akaike K, Hara K, Arakawa A, Takahashi M, et al. (2014) A case of dedifferentiated solitary fibrous tumor in the pelvis with Tp53 mutation. Virchows Arch 465: 615–621.
- Koelsche C, Schweizer L, Renner M, et al. (2014) Nuclear relocation of STAT6 reliably predicts NAB2-STAT6 fusion for the diagnosis of solitary fibrous tumour. Histopathology 65: 613–622.
- Travis WD, Brambilla E, Muller-Hermelink HK, Harris CC (2004) (Eds.): World Health Organization Classification of Tumours. Pathology and Genetics of Tumours of the Lung, Pleura, Thymus and Heart. IARC Press: Lyon.
- Khandelwal A, Virmani V, Amin MS, George U, Khandelwal K, et al. (2013) Radiology–pathology conference: malignant solitary fibrous tumor of the seminal vesicle. Clinical Imaging. 37: 409–413.
 LOGIN
LOGIN REGISTER
REGISTER.png)