Short Review
Cecilia Perin*
Department of Medicine and Surgery, Istituti Clinici Zucchi Hospital, Monza, Italy
*Corresponding author: Cecilia Perin, Department of Medicine and Surgery, Istituti Clinici Zucchi Hospital, Milano-Bicocca University, Piazza della Madonnina 1, Carate Brianza, Monza, Italy, Tel: +39 0362986205; Fax: +39 0362986; E-mail: cecilia.perin@unimib.it
Citation: Perin C (2017) The Influence of Personal Factors in Neurorehabilitation. Curr Adv Neurol Neurol Disord 2017: 5-8. doi: https://doi.org/10.29199/2637-6997/CANN-101014
Received: 09 July, 2017; Accepted: 15 August, 2017; Published: 31 August, 2017
Introduction
Disability emerging from trauma leads to a complete transformation of an individual’s existence, and has important consequences on quality of life. Studying the concerns resulting from traumatic events should involve an analysis of physical issues (International Classification of Functioning [ICF] - structure alteration), loss of function (ICF - body functions), limitations to activity and participation (ICF - performance and capacity), and consequent environmental and social arrangement (ICF - environmental) according to ICF classification model [1]. Furthermore, a multitude of individual factors, which, to date, have not been classified by ICF and termed “personal factors”, need to be considered.
Patients with neurological disorders distinguish from other rehabilitative conditions because generally physical changes preclude full recovery of a habitual working and relational lifestyle [2]. Fewer than one-half of working-age patients return to gainful employment because of residual disabilities after stroke. Analysis of functional scales has revealed that the outcomes appear to be even less positive for women [3]. Furthermore, physical limits can isolate the elderly, who risk receiving less rehabilitative care [4]. For these reason the assessment of an individual’s quality of life requires an analysis of daily and social activities, and psychological balance.
Most issues described in the literature have focused attention on the psychological functioning of the individual after a neurological event during the rehabilitation period. Depressive, anxious, and adaptive reactions have also been investigated, and often occur after an event and continue with a trend that is often difficult to modify. When an individual experiences a major stroke during working age, familiar social roles are often dismissed, and he/she will lose identity, confidence, and self-esteem. A review by Bays [5] focused attention on the lower of quality of life experienced after stroke with regard to what is expected in aging. Similar to the way elderly individuals with an active lifestyle slowly lose autonomy due to neurodegenerative disease, this may result in depression, isolation, and the loss of affective continuity. The same issues are also experienced by individuals living with other neurological conditions such as multiple sclerosis [6].
Challenging issues are also encountered by rehabilitation specialists when relating to individuals with physical, psychological, and/or neuropsychological deficits. Thus, in addition to typical techniques, the capacity to elaborate on emotion-focused and problem-focused strategies becomes essential. McKevitt et al., [7] assessed 95 qualitative studies involving stroke survivors and caregivers. This review revealed the communicative concerns between survivor and caregiver, and the lack of agreement regarding priorities. Furthermore, it stressed the importance of communication between the patient and operator for the resolution of practical and emotional issues [8,9].
The clinical experience that we described here is founded on the need to fully consider changes in a patient’s body, functioning, and lifestyle.
These changes are of different types, entity, and are disease-related and premorbid personality related:
- Disease-related psychiatric issues Psychiatric pathologies: the relationship between physical damage and psychiatric disorders has been widely explored. For example, the prevalence of depression in stroke patients varies from 20% to 60%. Post-traumatic stress disorder has been observed in 31% of individuals with major stroke [10]. Furthermore, hip fractures have been associated with an incidence of depression of approximately 7.5%, which becomes 50% in cases involving dementia. Our data outline that the presence of psychiatric disorders negatively impacts rehabilitative outcomes, and these appear to be more related to the existence of the trauma itself than to the type and severity of trauma [11].
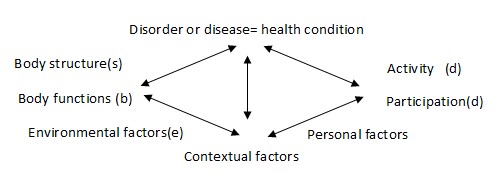
- Premorbid Personal factors involve sex and age, but also personality features, identity awareness and, potentially, 238 more factors [12]. Thanks to the efforts of the World Health Organization in creating ICF as a tool for describing individual functioning, this topic has attracted much attention. Defining ICF categories and their connection with personal features enables the development of a truly customized rehabilitation program (Figure 1).
|
Figure 1: Interaction between the components of the International Classification of Functioning model: disorders influence body function (b), and lead to modifications of activity and participation (d) that are also influenced by environmental (e) and personal factors. |
Attention is increasingly being devoted to premorbid personality, coping capacity, and self-esteem among the personal factors in many experimental studies.
Coping is defined as “the constantly changing in cognitive and behavioral efforts to manage the specific external or internal demands that are appraised as taxing or exceeding the resources of the person” [13]. More specifically, it is the modality with which individuals manage a serious and life-threating condition.
There are many examples of how coping strategies can help during the course of rehabilitation and in acceptance of quality of life. These strategies include the following: looking on the “bright side”; helping others; taking responsibility for self-care and decision making; slowing the pace of life; developing patience; developing routines; and staying motivated and active. These reaction modalities are included in the post-traumatic growth process, which leads to attainment of the best work-life balance - a healthier lifestyle known as “silver lining” [14].
Studies investigating coping modalities in stroke have reported that they do not change over time in a manner similar to personality traits [15]. Furthermore, studies examining
quality of life in patients with multiple sclerosis report that coping modalities are among the factors that determine individual wellness, and that they contribute to social isolation, family issues, and work complications [16]. In Parkinson’s disease, it has similarly been reported that increased attention to emotion-focused coping, with less focus on problem-focused coping, were determinants of quality of life, anxiety, and depression [17].
- Self-esteem involves the positive or negative evaluation of oneself, and has been found to be related to depression and anxiety [18]: self-esteem and efficacy attenuate depressive symptoms in chronic illness and increase reliance.
- Fewer current studies investigating premorbid personality area available. Studies investigating Traumatic Brain Injury (TBI) suggest that disinhibited aggressiveness emerges in individuals with pre-morbid aggressive behavior [19]. A major psychiatric comorbidity following TBI is associated with the type of pre-morbid personality [20]. In individuals with psychological symptoms of dementia [21], a neurotic personality is an important predictor of depression after stroke [22].
All of the above-mentioned features impact the relationship between the patient and the rehabilitation team. These aspects influence the environmental component (component “e” figure 1) of the ICF model, describing the suitability of services and social structures for the patient. The result is that healthcare professionals must now address disability more closely than ever previously. However, they have built impregnable defensive barriers, often concealed by an excessive emphasis on technical competencies, which can increase the risk for over-detachment from the environmental anguish surrounding their patients.
The relationship patient-rehabilitation team and the importance of personal factors in our experience:
We examined the question of whether is it possible to adopt tools that can facilitate the circulation of both rational and emotional content in such a way as to re-introduce the deepest parts of oneself; thus, making it possible to face a difficult and traumatic reality with an awareness of the limitations involved while simultaneously rediscovering life’s pleasures [9].
We introduced group conversations involving meetings between healthcare professionals and patients, followed by meetings among groups of healthcare professionals only. These prompts led to the creation of new associations and shared thoughts with the intervention of the group leader, who continuously proposed the themes and attempted to involve all of the participants.
The patient group was created according to the model proposed by Giampaolo Lai, the founder of It was, therefore, possible to discover the modalities through which patients share their experience of uneasiness and pain. Furthermore, it was possible to activate operators’ comprehension and participation, and to positively impact the patients’ capacity to react. In this work, items reflecting patient self-evolution and self-awareness have been observed. These have led other studies to focus on the role of the rehabilitative team on patients’ health improvement and on the importance of a relationship during rehabilitation management.conversationalism [23].
Furthermore, patient groups evolved in various directions:
- The formation of a group that speaks: compared with initiation, time and constancy permitted the creation of new relationships and a space in which the participants could exchange experiences;
- The elaboration of the dissociative process: participating in the group enabled patients to become aware of their situation and potential, which increased self-narration in terms of recounting their experiences before and after the traumatic event; and
- The formation of new key words: characterizing the experience of the participants.
This approach may help in finding a solution for issues such as challenging behavior. Using this definition, Brown [24] described behavioral difficulties, often features of TBI (but also of stroke) that arise from the interaction between an individual and the environment, including aggression, disinhibition, noncompliance, persistent screaming, disturbed behavior, and destructiveness. In addition, it has been possible to note an improvement in the control of emotional lability and catastrophic reaction, coexisting both in stroke and neurodegenerative diseases such as Parkinsonism. Furthermore, it has been observed that a patient’s self- and disease judgement can be attributed first to his/her cognitive skills, which in turn let him/her completely or partially be aware of his/her situation. Second, it may be a consequence of the psychological defense mechanism (e.g., denial; see ‘autobiographical accounts of stroke survivors-psychological management of stroke [25]).
Another component emerging from this experience was the importance of acceptance of self-body image. In a further study, we examined patients’ competence (capacity) to accept self-body malformation in a population of amputees (data in press). We explored coping-reaction modalities to self-body changes and noticed that prostheses were not fully integrated, and often it is used simply to appear in public and, therefore, relying only on the external aspect. Looking on his/her own shape traced with and without a prosthesis, many patients preferred to choose the complete one; however, this is not related to daily and functional use. Although many recognize the utility of the prosthesis, its use is very limited and is far from being perceived as part of themselves.
There is a correlation between the perception of disorder in their own image, and general and social adaption to the prosthesis, which influences the quality of life, specifically the limitations in physical and mental activity. This should be considered during the rehabilitation program. Undoubtedly, the rehabilitative setting needs to understand contextual factors (personal and environmental) during the formulation of goal planning as the elements that are involved in therapeutic success. The goal-setting process is a tool that promotes cohesion and facilitates communication, but relies on knowledge of personality, coping strategies, and awareness of the patient’s self-esteem.
The last step that guarantees comprehensive rehabilitation is patient involvement in the healthcare research process [26]. Patient participation in research is a patient-centered process that captures issues that patients, their relatives, clinical specialists, and researchers consider to be important. It has been suggested that this type of interdisciplinary research could be fixed on 7 goals, with characteristics focusing on participation and self-determination, a contextual approach, and the participation of disabled persons in participation research.
In conclusion, living with chronic illness is a complex, dynamic, cyclical, and multidimensional process, and involves the development of five different attributes: acceptance, coping, self-management, integration, and adjustment.
References
- World Health Organization (2001) International Classification of Functioning, Disability and Health. World Health Organization, Geneva, Switzerland.
- Knoflach M, Matosevic B, Rücker M, Furtner M, Mair A, et al. (2012) Functional recovery after ischemic stroke--a matter of age: data from the Austrian Stroke Unit Registry. Neurology 78: 279-285.
- Zalihi? A, Markoti? V, Dino Zalihi? D, Mabi? M (2010) Gender and quality of life after cerebral stroke. Bosnian J Basic Med Sci 10: 94-99.
- Bentsen L, Christensen L, Christensen A, Christensen H (2014) Outcome and risk factors presented in old patients above 80 years of age versus younger patients after ischemic stroke line Bentsen.
J Stroke Cerebrovasc Dis 23: 1944-1948. - Bays CL (2001) Older adult’s descriptions after stroke. Rehabil Nurs 26: 18-20, 23-27.
- Fiest KM, Walker JR, Bernstein CN, Graff LA, Zarychanski R, et al. (2016) Systematic review and meta-analysis of interventions for depression and anxiety in persons with multiple sclerosis. Mult Scler Relat Disord 5: 12-26.
- Mckevitt C, Redfern J, Mold F, Wolfe C (2004) Qualitative studies of stroke: a systematic review. Stroke 35: 1499-1505.
- Wachters-Kaufmann CSM (2000) Personal accounts of stroke experiences. Patient Educ Couns 41: 295-303.
- Perin C, Beghi M, Cerri CG, Peroni F, Viganò B (2015) Experience of group conversations in rehabilitation medicine: methodological approach and pilot study. J Med Pers 13: 96-104.
- Robinson RG (2003) Poststroke depression: prevalence, diagnosis, treatment, and disease progression. Biol Psychiatry 54: 376-387.
- Meroni R, Beghi E, Beghi M, Brambilla G, Cerri C et al. (2013) Psychiatric disorders in patients suffering from an acute cerebrovascular accident or traumatic injury, and their effects on rehabilitation: an observational study. Eur J Phys Rehabil Med 49: 31-39.
- Geyh S, Peter C, Müller R, Bickenbach JE, Kostanjsek N, et al. (2011) The personal factors of the international classification of functioning, disability and health in the literature - a systematic review and content analysis. Disabil Rehabil 33: 1089-1102.
- Lazarus RS, Folkman S (1984) Stress, appraisal and coping. Springer, New York, USA.
- Gangstad B, Norman P, Barton J (2009) Cognitive processing and posttraumatic growth after stroke. Rehabil Psychol 54: 69-75.
- Donnellan C, Hevey D, Hickey A, O’Neill D (2006) Defining and quantifying coping strategies after stroke: a review. J Neurol Neurosurg Psychiatry 77: 1208-1218.
- Lysandropoulos AP, Havrdova E, ParadigMS Group (2015) ‘Hidden’ factors influencing quality of life in patients with multiple sclerosis. Eur J Neurol 22: 28-33.
- Garlovsky JK Overton PG, Simpson J (2016) Psychological predictors of axiety and depression in Parkinson’s disease: a systematic review. J Clin Psychol 72: 979-998.
- Vickery CD, Evans CC, Lee JE, Sepehri A, Jabeen LN (2009) Multilevel modeling of self-esteem change during acute inpatient stroke rehabilitation. Rehabil Psychol 54: 372-380.
- Greve KW, Sherwin E, Stanford MS, Mathias C, Love J, et al. (2001) Personality and neurocognitive correlates of impulsive aggression in long-term survivors of severe traumatic brain injury. Brain Inj 15: 255-262.
- Rogers JM, Read CA (2007) Psychiatric comorbidity following traumatic brain injury. Brain Inj 21: 1321-1333.
- Low LF, Brodaty H, Draper B (2002) A study of premorbid personality and behavioural and psychological symptoms of dementia in nursing home residents. Int J Geriat Psychiatry 17: 779-783.
- Storor DL, Byrne GJ (2006) Premorbid personality and depression following stroke. Int Psychogeriat 18: 457-469.
- Lai G (1985) La conversazione felice. Il Saggiatore, Milano, Italy. Pg no: 215.
- Brown AW, Moessner AM, Mandrekar J, Diehl NN, Leibson CL, et al. (2011) A survey of very-long-term outcomes after traumatic brain injury among members of a population-based incident cohort. J Neurotrauma 28: 167-176.
- Lincoln NB, Kneebone II, Macniven JAB, Morris RC (2012) Conclusions and Future Directions. In: Lincoln NB, Kneebone II, Macniven JAB, Morris RC (eds.). Psychological Management of Stroke. (1st edn), John Wiley & Sons, New Jersey, USA. Pg no: 486-487.
- Farin E, Arbeitsgruppe, Teilhabeforschung“ des Ausschusses, Reha-Forschung“ der Deutschen Vereinigung für Rehabilitation und der Deutschen Gesellschaft für Rehabilitationswissenschaften (2012) [Discussion paper participation research]. Rehabilitation (Stuttg) 51: 28-33.
 LOGIN
LOGIN REGISTER
REGISTER.png)